¿Por qué el tratamiento de IVF es tan popular?
Ten years ago, not everyone was familiar with IVF and its use to treat infertility. For better or for worse, the news of the Octomom in those days brought much awareness to this assisted reproductive technology. In that specific case, it showed us what NOT to do when it comes to the use of this treatment: transferring too many embryos.
To date there have been over 3 million births around the world from In-Vitro Fertilizations since the procedure became available in 1978. Its popularity is due to its effectiveness as it provides the highest success rates when treating infertility.
What happens during an IVF treatment?
The patient is usually placed on birth control pills to regulate her menstrual cycles. Medications such as injectable gonadotropins that stimulate your ovaries and follicle growth are added at this time depending on the protocol your fertility specialist chooses. Once you stop taking birth control pills, injectable gonadotropins will be used to stimulate as many eggs as safely as possible. You will have transvaginal ultrasounds performed to monitor the growth of the follicles, usually about 3-5 times once the birth control pills are stopped. Once the lead follicles reach a size of around 18-22mm, then the hCG trigger will be given. About 35 hrs after the trigger, you will be taken to a surgical suite, and using the same transvaginal ultrasound, a needle (same type used to draw blood, but longer) is “poked” through the vagina (with the ultrasound probe looking straight into the ovary) and the needle placed directly into the follicle. Under suction, the contents of the follicle are removed and go into a test tube (hence the old name “test tube babies”). The eggs are taken out of the test tubes and placed into a Petri Dish where the sperm are placed with the egg for fertilization. The embryos are incubated for 3-5 days. The resulting embryos on a daily basis are checked to make sure theyre diving properly and “graded”. At the day of transfer, depending on the embryos cellular division and quality, your fertility specialist and you will decide how many will be transferred back. Please note there are guidelines provided by the American Society for Reproductive Medicine in terms of how many embryos are safe to transfer. Most patients elect one or two embryos.
The embryos are placed into a catheter, the fertility specialist will then place a speculum just like a pap smear, the catheter containing the embryos are passed through the cervix and into the uterus where they’re deposited. Progesterone and Estrogen will be taken thereafter and a blood hCG level is drawn about 12 days after egg retrieval.
One of the advantages of IVF is the amount of technologies available to be used along with this treatment to increase your chances of pregnancy. These are the most common technologies that are available to those who are undergoing In Vitro Fertilization (IVF):
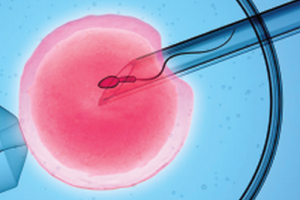
Intracytoplasmic Sperm Injection (ICSI)
This is a procedure in which a single sperm is isolated and directly injected into the egg, creating fertilization. This technique was revolution when finally mastered in the late 1990s. Prior to this, men who produced few sperm or sperm with low morphology (shape) or motility (swimmers), required donor sperm since their sperm may not have had the capacity of burrowing through the eggs shell appropriately. With ICSI, we dont have to worry about burrowing through the eggs shell, as a syringe will contain a single sperm and this is directly injected into the egg and as stated above, fertilization is achieved.
Egg freezing (Oocyte Cryopreservation)
CARE Fertility is also proud to provide egg freezing with IRB approval from the Glendale Adventist Medical Center as recommended by the American Society for Reproductive Medicine (ASRM). Under FDA regulations, an IRB is an appropriately constituted group that has been formally designated to review and monitor biomedical research involving human subjects. Eggs (Oocyte) are placed on a special freezing environment. They can remain frozen for months or even years, and can be thawed for use in IVF in the future.
Testicular Sperm Extraction (TESE)
Usually performed by a Urologist who specializes in Male Fertility. Approximately 40% of men who produce no sperm have some sort of tubal obstruction (yep, sperm have to pass through a series of pipes to be ejaculated) usually in the Vas Deference. Men who have had hernia repairs are usually at high risk for having obstructions created from surgery. Some men, especially those with mild forms of Cystic Fibrosis are born without the Vas Deference (partner testing will be required). In these cases, there is usually ample sperm in the testis (epididymis). A Urologist can simply extract sperm directly from the testis with a special syringe. The eggs extracted from IVF can then be fertilized via ICSI using these sperm.
Embryos sometimes have shells that surround them that look very thick. We believe that these thickened shells may not allow the embryo to hatch sometimes, which wouldnt allow for implantation and pregnancy. These thickened shells are notoriously encountered in Poor Responders and in women over the age of 38. The shell can be thinned out either with a laser or an acid solution to make it easier for the embryo to hatch.
Preimplantation Genetic Diagnosis (PGD)
A procedure where a specific genetic defect can be determined in embryos. A Day 3 embryo usually has 8 cells and one of these cells is extracted and analyzed for the specific defect. For example, a couple both are carriers for Cystic Fibrosis (CF), meaning they are at high risk for passing CF to their children. The cell that was extracted from the embryo is analyzed for CF, and if the cell doesnt have this genetic defect, it is assumed the embryo does not and vice versa. Only those embryos that had the normal cells would then be transferred back into the uterus to allow implantation and pregnancy to occur with a non-afflicted baby.
Nowadays, sometimes when a family has a child that has a certain type of leukemia and there is no one in the family with a bone marrow match, couples may undergo IVF + PGD to specifically look for an embryo that will carry a bone marrow match. Once the embryo(s) are identified, these embryos are transferred back. Once this baby is born, a small sample of the babys bone marrow is taken to save his/her siblings life from leukemia.
Preimplantation Genetic Screening (PGS)
A procedure in which couples simply want to make sure the embryos being transferred back are chromosomally normal. The biopsy can either be performed on Day 3 or Day 5 blastocysts (embryo). The advantage of doing a day 5 trophoectoderm biopsy is that multiple cells (not just one that is done on Day 3) can be biopsied, usually from the area of the blastocysts that is destined to be the placenta. Presently, there are two ways to screen embryos, either through Flourescent In-Situ Hybridization (FISH) or Comparative Genetic Hybridization (CGH). FISH can not check all of the chromosomes, so only a few are checked. CGH can check all 46 (including sex) chromosomes and is becoming commercially available. Both of these procedures only check for the number of chromosomes, which can avoid genetic defects such as Downs Syndrome. With a Day 3 transfer, the resulting fresh blastocyst can be transferred back fresh on Day 5. If one desires to do CGH, the biopsied embryo must presently be frozen because it takes a few weeks to get the results back. Then, the normal embryos are thawed and transferred back. As several articles are pointing out however, the biopsied cells that are being screened with these two technologies are not necessarily representative of the cell itself. Some abnormal embryos seem to self-correct and become normal babies and vice versa. Pregnancy rates also appear to be lower when the embryos are biopsied like this. Although CGH is more complete than FISH for checking chromosomes, CGH is in its infancy and requires at present the freezing of the biopsied blastocyst with eventual thawing of the normal blastocyst for transfer. At present, PGS remains controversial in the fertility world, and is not presently recommended by the community for simple screening purposes.
Microarray Chips are presently under scientific investigation in which several hundreds of genes (not just the chromosome number) can be evaluated in each embryo. Lethal and/or debilitating genes found in embryos can primarily be evaluated and only those that do not carry these genes can be transferred, but this technology is still a few years away from being commercially available.
There are still many more technologies being developed, such as finding embryo markers in culture media that by simply checking the media and not manipulating the embryo, we may be able to determine the best embryo. Others are studying flow dynamics to try and mimic the fallopian tube environment for the embryo. Whereas these make sense, we are hopeful that within a few years, we will be able to provide these technologies to you to not only improve pregnancy rates, but to also provide diagnosis when needed.
At CARE Fertility, we’re committed to helping you overcome infertility. We offer a first free consultation with one of our board certified fertility specialists to help you determine if IVF is the best treatment for you.
